Τι είναι η Ολική Αρθροπλαστική Ισχίου (THA);
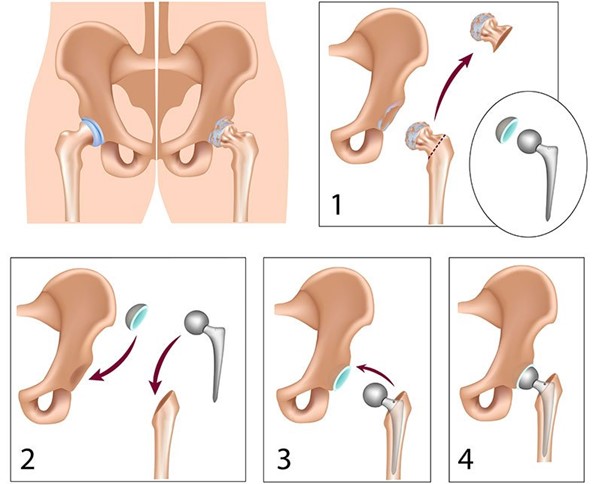
Στην προχωρημένη αρθρίτιδα του ισχίου, ο χόνδρος (το λείο κάλυμμα του οστού) καταστρέφεται και η κίνηση γίνεται επώδυνη όσο και αδύνατη. Η άρθρωση του ισχίου αποτελείται από τη μηριαία κεφαλή η οποία είναι σφαιρική και αρθρώνεται (συνδέεται) με μια υποδοχή στη λεκάνη, που ονομάζεται κοτύλη. Στο THA, η κεφαλή αφαιρείται και αντικαθίσταται με πρόσθεση και ταυτόχρονα η κοτύλη διαμορφώνεται κατάλληλα ώστε να δέχεται ένα εμφύτευμα που μοιάζει με ημισφαιρική υποδοχή και ταιριάζει στη μεταλλική κεφαλή. Ένα πλαστικό ένθετο τοποθετείται μεταξύ της κεφαλής και της εσοχής που μειώνει τις δυνάμεις τριβής. Στην Αγγλία γίνονται περισσότερες από 70.000 OAI ετησίως και τηρείται αναλυτικό αρχείο.
Πότε είναι ΘΑ υποδεικνύεται:
- Όταν η άρθρωση είναι αρθριτική
- Ο πόνος επηρεάζει την ποιότητα ζωής καθιστώντας τον αφόρητο (π.χ. αδυναμία βάδισης) ακόμη και με παυσίπονα ή ακόμα και διακόπτει τον ύπνο
- Υπάρχει δυσκαμψία και δυσκολία στην κίνηση
- Η αναλγησία (παυσίπονα) δεν ελέγχουν πλέον τα συμπτώματα
Το THA αντενδείκνυται όταν έχουμε:
- Ενεργή λοίμωξη κοντά στο ισχίο.
- Πολύ κακή κατάσταση κυκλοφορίας στα κάτω άκρα
- Όταν ο περιεγχειρητικός κίνδυνος είναι πολύ υψηλός και υπερτερεί των οφελών/ασθενείς υψηλού κινδύνου
- Στα αρχικά στάδια της αρθρίτιδας όταν ο πόνος είναι ήπιος
Πρέπει να πάω για THA;
Αυτό είναι κάτι που θα σας συστήσει ο ειδικός γιατρός με βάση τα συμπτώματα και το ιστορικό σας και θα αποφασίσετε σταθμίζοντας τα συμπτώματά σας, τους κινδύνους και τα οφέλη της επέμβασης. Ο Δρ Κ. Ευαγγέλου θα χαρεί να απαντήσει σε οποιαδήποτε απορία σας.
Ποια υλικά είναι καλύτερα; Υπάρχουν απαρχαιωμένα υλικά;
Η επανάσταση της αρθροπλαστικής ισχίου ξεκίνησε και συνεχίστηκε στην Αγγλία. Σκοπός αυτής της μεγάλης επέμβασης είναι η εξάλειψη του πόνου με τις λιγότερες δυνατές επιπλοκές, αποκαθιστώντας παράλληλα την ανατομία του ισχίου. Ταυτόχρονα θα πρέπει να έχει διάρκεια ζωής τουλάχιστον 15 -20 χρόνια με καλή λειτουργική έκβαση.
Τα καλύτερα υλικά είναι αυτά που λειτουργούν στα χέρια του χειρουργού σας, σέβονται το οστό, αποκαθιστούν την ανατομία και ταυτόχρονα εξασφαλίζουν καλή λειτουργία για χρόνια βάσει μελετών. Ο χειρουργός σας θα συστήσει τα καλύτερα εμφυτεύματα με βάση την ηλικία, τις ανάγκες και το ιστορικό σας. Κάθε ασθενής είναι διαφορετικός.
Πόσοι τύποι OAI υπάρχουν;
Ιστορικά, οι κύριες κατηγορίες εμφυτευμάτων OAI είναι εκείνα που στερεώνονται με οστικό τσιμέντο και εκείνα που εμφυτεύονται στο μηριαίο κανάλι με τρόπο πίεσης. Μπορούν όμως να διακριθούν με βάση τα υλικά, το μέγεθος της τομής ή τη βοήθεια του χειρουργού από ένα ρομποτικό μηχάνημα.
Πόσο διαρκεί μια αντικατάσταση ισχίου;
Όλα τα υλικά είναι επιρρεπή στη φθορά. Τα εμφυτεύματα ολικής αντικατάστασης ισχίου έχουν σχεδιαστεί για να διαρκούν τουλάχιστον 15 χρόνια. Συχνά μια αντικατάσταση ισχίου διαρκεί 20 έως 30 χρόνια. Για άλλους, ένα τεχνητό ισχίο μπορεί να φθαρεί και να χρειαστεί αντικατάσταση νωρίτερα.
Πολλοί παράγοντες συμβάλλουν στη διάρκεια ζωής ενός τεχνητού ισχίου συμπεριλαμβανομένου του ασθενούς: φυσική κατάσταση, επίπεδο σωματικής δραστηριότητας και βάρος.
Τι ποσοστά επιτυχίας έχει ο ΟΑΙ;
- Τα ποσοστά επιτυχίας αγγίζουν το 97%
- Οι ασθενείς θα παρατηρήσουν την εξάλειψη του αρθριτικού πόνου και τη βελτίωση της κίνησης
- Το περπάτημα επιτρέπεται άμεσα υπό την επίβλεψη εξειδικευμένου φυσιοθεραπευτή
Τι περιλαμβάνει μια επιτυχημένη προεγχειρητική αξιολόγηση;
- Συμβουλέψτε τους ασθενείς να βελτιώσουν τη φυσική τους κατάσταση
- Απώλεια βάρους/ Συμβουλέψτε τους ασθενείς να μειώσουν το BMS τους
- Αναισθητική ανασκόπηση βασισμένη σε προηγούμενο Καρδιολογικό ιστορικό
- Βελτιστοποίηση των επιπέδων σακχάρου στο αίμα
- Θεραπεία οποιασδήποτε πιθανής λοίμωξης (π.χ. λοίμωξη που σχετίζεται με τα δόντια, το δέρμα και ειδικά στα πόδια ή τα ούρα)
- Εξετάσεις αίματος και πλήρες ιστορικό, ΗΚΓ και ακτινογραφίες
Ποιοι είναι οι σοβαροί κίνδυνοι στον ΟΑΙ;
Γενικά κάθε ιατρική πράξη έχει σχετικούς κινδύνους.
- Λοίμωξη (παρά τα αντιβιοτικά τα ποσοστά είναι μικρότερα από 1/100 χειρουργικές επεμβάσεις. Η σοβαρή λοίμωξη του ισχίου δεν μπορεί να αντιμετωπιστεί μόνο με αντιβιοτικά και μπορεί να απαιτήσει αφαίρεση και εκ νέου εμφύτευση εμφυτευμάτων.
- Θρόμβοι κάτω άκρων (εν τω βάθει φλεβική θρόμβωση). Είναι μια σπάνια αλλά υπάρχουσα επιπλοκή. Οι ασθενείς συνήθως λαμβάνουν αντιπηκτικά 1 μήνα μετά την επέμβαση, κινητοποιούνται και ενυδατώνονται άμεσα. Ωστόσο, δεν μπορούν να αποφευχθούν όλοι οι θρόμβοι αίματος. Σπάνιες (1/1600 περιπτώσεις ή 0,06% παρουσιάζουν θανατηφόρα πνευμονική εμβολή.
- Εξάρθρημα ισχίου
- Ασυμφωνία μήκους ποδιού
- Άσηπτη χαλάρωση εμφυτευμάτων λόγω υπολειμμάτων φθοράς μετά από χρόνια (5/100 περιπτώσεις).
Γίνονται οι διαδικασίες THA κατά τη διάρκεια της πανδημίας COVID-19;
Ο κ. Κ. Ευαγγέλου έχει ολοκληρώσει την υποτροφία του στη Μεγάλη Βρετανία και έχει εργαστεί εδώ κατά τη διάρκεια της πανδημίας. Μετά την πρώτη φάση της πανδημίας την άνοιξη του 2020, όλες οι προαιρετικές χειρουργικές δραστηριότητες πραγματοποιήθηκαν κανονικά. Με την εφαρμογή των ασφαλέστερων πρωτοκόλλων που χρησιμοποιούνται στο Ηνωμένο Βασίλειο, μπορεί να πραγματοποιηθεί με ασφάλεια ένα THA κατά τη διάρκεια της πανδημίας
