What is Total Hip Arthroplasty (THA)?
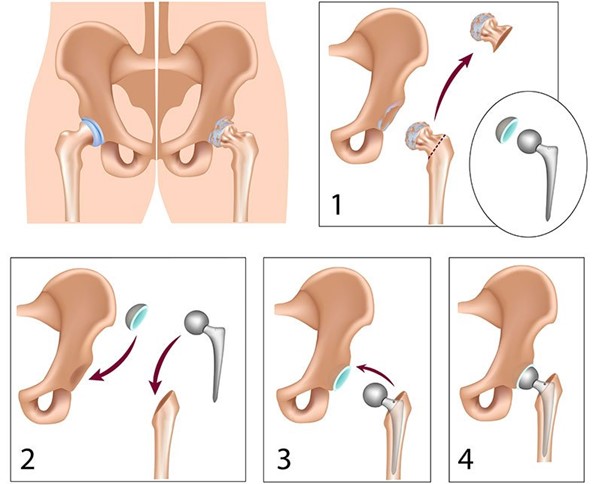
In advanced hip arthritis, the cartilage (the smooth covering of the bone) is destroyed and movement becomes painful as well as impossible. The hip joint consists of the femoral head which is spherical, and is articulated (connected) to a socket in pelvis, called the acetabulum. In THA, the head is removed and replaced with a prosthesis and at the same time the acetabulum is properly reamed to accept an implant that looks like a hemispherical socket and fits the metal head. A plastic insert is placed between the head and the recess that reduces the frictional forces. In England more than 70,000 OAIs are made per year and a detailed file is kept.
When is THA indicated:
- When the joint is arthritic
- The pain affects the quality of life by making it unbearable (eg inability to walk) even with painkillers or even interrupts sleep
- There is stiffness and difficulty in movement
- Analgesia (painkillers) no longer control the symptoms
THA is contraindicated when we have:
- Active infection near the hip.
- Very poor condition of circulation in the lower extremities
- When the perioperative risk is very high and outweighs the benefits/high risk patients
- At the early stages of arthritis when the pain is mild
Do I have to go for a THA?
This is something that the specialist doctor will recommend based on your symptoms and history and you will decide by weighing your symptoms, risks and benefits of the operation. Dr. K. Evangelou will be happy to answer any of your questions.
Which materials are better? Are there outdated materials?
The revolution of hip arthroplasty began and continued in England. The purpose of this major operation is to eliminate pain with the fewest possible complications, while restoring the anatomy of the hip. At the same time it should have a lifespan of at least 15 -20 years with good functional outcome.
The best materials are those that work in the hands of your surgeon, respect the bone, restore the anatomy and at the same time ensure good function for years based on studies. Your surgeon will recommend the best implants based on your age, needs and history. Every patient is different.
How many types of OAI are there?
Historically, the major categories of OAI implants are those that are fixed with bone cement and those that are implanted into the femoral canal in a press fit manner. But they can be distinguished based on materials, the size of the incision or the assistance of the surgeon by a robotic machine.
How long does a hip replacement last?
All material are prone to wear. Total Hip Replacement implants are designed to last for at least 15 years. Often a hip replacement will last 20 to 30 years. For others, an artificial hip may wear and need replacing sooner.
Many factors contribute to the lifespan of an artificial hip including the patient’s: physical condition, level of physical activity and, weight.
What success rates does OAI have?
- Success rates reach 97%
- Patients will notice the elimination of arthritic pain and improvement of movement
- Walking is allowed immediately under the supervision of a specialized physiotherapist
What does a successful pre –operative assessment includes?
- Advise patients to improve fitness
- Weight loss/ Advise patients to reduce their BMS
- Anaesthetic Review based on previous Cardiac history
- Optimization of blood sugar levels
- Treatment of any possible infection (eg tooth associated infection, skin and especially in the feet, or urine)
- Blood tests and complete history, ECG and x-rays
What are the serious risks in OAI?
Generally every medical procedure has relative risks.
- Infection (despite antibiotics the rates are less than 1/100 surgeries. Serious hip infection can not be treated with antibiotics only and may require removal and re-implantation of implants.
- Lower extremity clots (deep vein thrombosis). It is a rare but existing complication. Patients usually receive anticoagulants 1 month after surgery, mobilise and are hydrated immediately. However, not all blood clots can be avoided. Rare (1/1600 cases or 0.06% present with fatal pulmonary embolism.
- Hip dislocation
- Leg Length Discrepancy
- Aseptic loosening of implants due to wear debris after years (5/100 cases).
Are THA procedures performed during the COVID-19 pandemic?
Mr K. Evangelou has completed his fellowship training in Great Britain and has worked here during the pandemic. Following the first phase of the pandemic in Spring 2020, all elective surgical activities were carried out as normal. By implementing the safest protocols used in UK, a THA can be safely performed during the pandemic
